Jacqueline Lewis is now raising her 7-year-old granddaughter; the child’s father, Shaun Lewis, died of a drug overdose this fall. There are thousands of similar “grandfamilies” in the U.S. Lewis believes those families should have a voice in determining how the settlement money from cases against opioid manufacturers and distributors are spent.
Maddie McGarvey for KHN
hide caption
toggle caption
Maddie McGarvey for KHN
With more than 200 Americans still dying of drug overdoses each day, states are beginning the high-stakes task of deciding how to spend billions of dollars in settlement funds from opioid manufacturers and distributors. Their decisions will have real-world implications for families and communities across the country that have borne the brunt of the opioid crisis.
Will that massive tranche of money be used to help the people who suffered the most and for programs shown to be effective in curbing the epidemic? Or will elected officials use the money for politically infused projects that will do little to offer restitution or help those harmed?
Jacqueline Lewis, of Columbus, Ohio, is wondering exactly that. She lost her son, Shaun, this fall after his 20-year struggle with addiction.

Shaun Lewis died in October 2022 at age 34 after wrestling with an addiction to opioids for 20 years. He was first prescribed the painkillers in middle school.
Maddie McGarvey for KHN
hide caption
toggle caption
Maddie McGarvey for KHN

Shaun Lewis died in October 2022 at age 34 after wrestling with an addiction to opioids for 20 years. He was first prescribed the painkillers in middle school.
Maddie McGarvey for KHN
After emptying her retirement account and losing her house to pay for his rehab, court fees, and debts to dealers, Lewis is now raising her 7-year-old granddaughter while also caring for her 95-year-old mother with dementia, on nothing more than Social Security payments.
When she heard Ohio would receive $808 million in opioid settlement funds, Lewis thought there’d finally be relief for thousands of families like hers.
She was eager to speak with members of the OneOhio Recovery Foundation, which was created to oversee the distribution of most of Ohio’s funds. As they determined priorities for funding, she wanted them to consider perspectives like hers — that of a mother and grandmother who’d faced addiction up close and saw the need for more treatment centers, addiction education in the workplace, and funding for grandparents raising grandkids as a result of the opioid epidemic.
But she couldn’t find anyone to listen. At an August foundation meeting she attended, board members excused themselves to go into a private session, she said. “They just left the room and left us sitting there.” When she attended another meeting virtually, audience members weren’t allowed to “voice anything or ask questions.”
A local group that advocates for people affected by the opioid epidemic has expressed similar concerns about the lack of opportunities for the public to speak with the foundation. That group is now suing the foundation for a lack of transparency, even though few decisions about funding priorities have been made yet.
Each state has its own approach to spending
The strife in Ohio highlights the tensions emerging nationwide as settlement funds start flowing. The funds come from a multitude of lawsuits, most notably a $26 billion settlement resulting from more than 3,000 cities, counties, and states suing manufacturer Johnson & Johnson and distributors McKesson, AmerisourceBergen, and Cardinal Health for their roles in the opioid crisis.
Payments from that case began this summer and will continue for 18 years, setting up what public health experts and advocates are calling an unprecedented opportunity to make progress against an epidemic that has ravaged America for three decades.
But, they caution, each state seems to have its own approach to these funds, including different distributions between local and state governments and various processes for spending the money. With countless individuals and groups advocating for their share of the pie — from those dealing with addiction and their families to government agencies, nonprofits, health care systems and more — the money’s impact could depend heavily on geography and politics.
“It sounds like a lot of money, but it’s going to a lot of places and going to be spread out over time,” said Sara Whaley, a researcher at Johns Hopkins Bloomberg School of Public Health who tracks state use of opioid funds. “It’s not going to magically end this crisis. But if it’s used well and used thoughtfully, there is an opportunity to make a real difference.”
And if not, it could be just another political boondoggle.
How to avoid the ‘tobacco nightmare’
The worst-case scenario, many say, is for the opioid settlement to end up like the tobacco master settlement of 1998.
States won $246 billion over 25 years, but less than 3% of the annual payouts are used for smoking prevention or cessation programs, according to the Campaign for Tobacco-Free Kids. Most has gone toward filling budget gaps, building roads and subsidizing tobacco farmers.
But there are stronger protections in place for the opioid settlement dollars, said Christine Minhee, founder of a website that tracks the funds.
The arrangement specifies that states must spend at least 70% of the money for opioid-related expenses in the coming years and includes a list of qualifying expenses, like expanding access to treatment and buying the overdose reversal medication naloxone. Fifteen percent of the funds can be used for administrative expenses or to reimburse themselves for past opioid-related expenses. Only the remaining 15% can be spent any way the states choose.
If states don’t meet those thresholds, they could face legal consequences and even see their future payouts reduced, Minhee said.
“The kind of tobacco nightmare stuff where only 3% of funds were spent on what they were meant for is legally and technically impossible,” she said. Though, she added, “a different nightmare is still possible.”
Experts tracking the funds say transparency around who receives the money and how those decisions are made is key to a successful and useful distribution of resources.
In Rhode Island, for instance, public comment is a regular part of opioid advisory committee hearings. In North Carolina and Colorado, online dashboards show how much money each locality is receiving and will track how it is spent.
But other states are struggling.
Mistrust grows when there’s little public input
In Ohio, the document that creates a private foundation to oversee most of the state’s funds says that “the Foundation shall operate in a transparent manner” and that meetings and documents will be public. Yet the OneOhio Recovery Foundation has since said it is not subject to open-meetings law. It has adopted a policy that meetings can be closed if the board decides the content is “sensitive or confidential material that is not appropriate for the general public.”
The contradiction between the board’s actions and how it was conceived led Dennis Cauchon, president of Harm Reduction Ohio, which distributes naloxone across the state, to sue the foundation. He said he wants the public to have more say in how the funding is spent.
“The board members are in a closed loop, and they’re having a hard time learning what the needs are,” Cauchon said.

Dennis Cauchon is president of Harm Reduction Ohio. His organization has taken legal action to press for more public input and and transparency in how the state’s opioid settlement funds are distributed.
Maddie McGarvey/Maddie McGarvey for KHN
hide caption
toggle caption
Maddie McGarvey/Maddie McGarvey for KHN

Dennis Cauchon is president of Harm Reduction Ohio. His organization has taken legal action to press for more public input and and transparency in how the state’s opioid settlement funds are distributed.
Maddie McGarvey/Maddie McGarvey for KHN
The 29-member board includes representatives of local regions, as well as appointees from the governor, state attorney general and legislative leaders. Many are city- and county-level politicians, and one is the wife of a U.S. senator. They are not paid for their service as board members.
Nathaniel Jordan, executive director of the nonprofit Columbus Kappa Foundation, which distributes naloxone to Black communities in Ohio, has raised concerns about the board’s lack of racial diversity. Since 2017, Black men have had the highest rate of drug overdose deaths in the state, he said, but only one board member is Black. “What gives?”
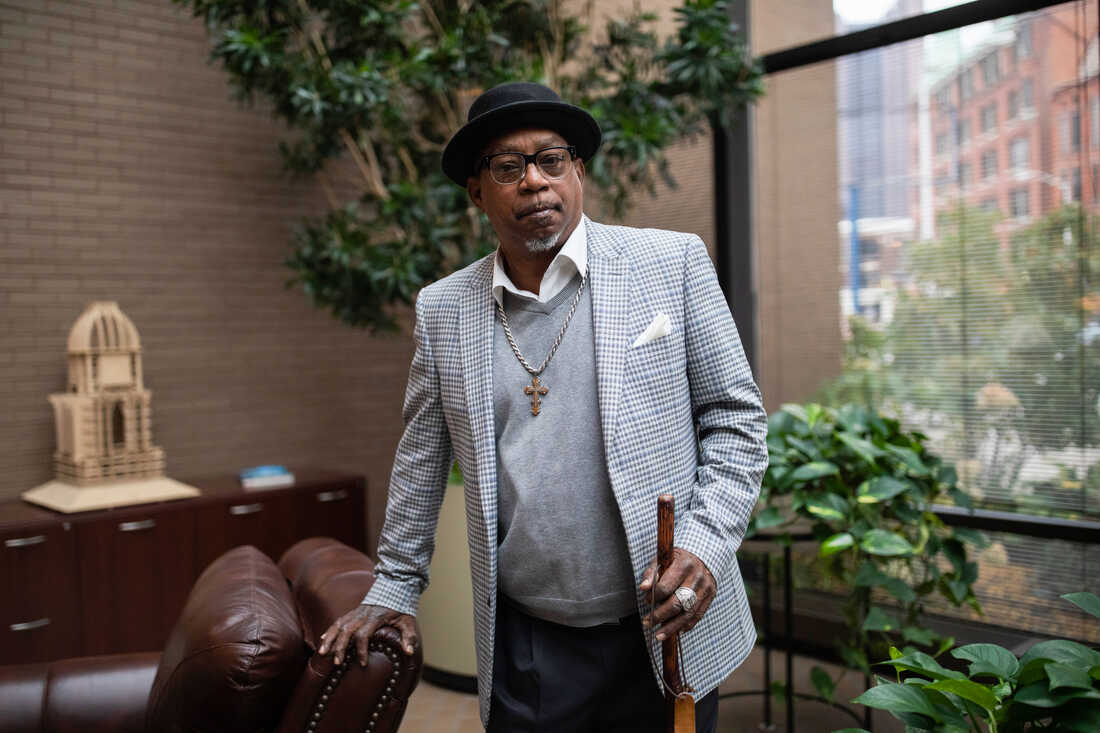
Nathaniel Jordan heads the Columbus Kappa Foundation, a nonprofit that distributes naloxone within hard-hit Black communities in Ohio. He’s concerned that the 29-person board of directors of the OneOhio Recovery Foundation includes just one Black member.
Maddie McGarvey for KHN
hide caption
toggle caption
Maddie McGarvey for KHN

Nathaniel Jordan heads the Columbus Kappa Foundation, a nonprofit that distributes naloxone within hard-hit Black communities in Ohio. He’s concerned that the 29-person board of directors of the OneOhio Recovery Foundation includes just one Black member.
Maddie McGarvey for KHN
Kathryn Whittington, chair of the OneOhio Recovery Foundation, said the board is being “very transparent in what we are doing.” The public can attend meetings in person or online. Recordings of past meetings are posted online, along with the agenda, board packet, and policies discussed — including a draft of the diversity and inclusion policy the board is considering.
People who want to provide input “can always reach out to me as the chair or any other board member,” said Whittington, who added that two of her children have struggled with addiction. But the best option, she said, is to contact one of Ohio’s 19 regional boards. Those groups can elevate local concerns to the foundation board.
“We are still at the very beginning,” Whittington emphasized. No money from the 18-year settlement has been spent yet. The board’s operational expenses — including a $10,000-per-month contract with a public relations firm — is being paid out of $1 million from a previous opioid-related settlement.
But Lewis, the woman raising her granddaughter in Columbus, worries that the day for families to speak may never come.
“They keep saying it’s not ready, and before you know it, they’ll be handing out money and it’ll be too late,” she said.
Rhode Island will spend $2 million on a site where drug use is supervised
Rhode Island is one of the states working fastest to distribute settlement dollars. Its Executive Office of Health and Human Services, which controls 80% of the funds and works with an opioid advisory committee, released a plan to use $20 million by July 2023.
Although the plan doesn’t specify funding for people raising grandchildren, it does allocate $900,000 to recovery supports, which will include community agencies that serve family members, the department said. The single largest allocation, $4 million, will go to school-and community-based mental health programs.
The investment that has sparked the most interest in Rhode Island is $2 million for a supervised drug consumption site. Its location and opening date will be determined by organizations that respond to the state’s request for proposals, said Carrie Bridges Feliz, chair of the opioid settlement advisory committee. At a time when fentanyl, a synthetic opioid that is up to 50 times stronger than heroin, is infiltrating most street drugs and overdose rates are high, “we were anxious to make use of these funds,” Bridges Feliz said.
Louisiana plans to give 20% of its share to sheriffs
In contrast, the process of distributing settlement dollars in Louisiana has barely begun. State Attorney General Jeff Landry announced in July 2021 that Louisiana was expected to receive $325 million from the 18-year settlement but has not released any additional information. His office did not respond to repeated inquiries about the status of the funds.
The governor’s office and state health department said they could not answer specific questions about the funds and had not yet been contacted by the attorney general’s office, which negotiated the state’s settlement agreement. Multiple clinicians who treat substance use disorder and advocates who work with people who use drugs were similarly in the dark.
The state’s written plan says it will create a five-person task force to recommend how to spend the money. Kevin Cobb, president of the Louisiana Sheriffs’ Association, said the group had appointed its representative to the task force, but he didn’t know if other members had been selected or when they would meet.
One decision Louisiana has made so far is to give 20% of the settlement funds directly to sheriffs — a move that has made some people nervous.
“This plays into an increase in support for an authoritarian response to what are public health issues,” said Nadia Eskildsen, who has worked for syringe service programs and other such groups in New Orleans.
She worries that the money will be funneled toward increasing arrests, rather than helping people find housing, work or health care. Meanwhile, almost 1,400 Louisiana residents died of opioid-related causes last year.
K.P. Gibson, the Acadia Parish sheriff who will represent the sheriffs’ association on the state task force, said his focus is not on punishment, but on getting people into treatment. “My jail problem will resolve itself if we resolve the problem of opioid addiction,” he said.
Many health and policy experts say using settlement funds to pair mental health professionals with police officers or provide medications for opioid use disorder in prisons could reduce deaths.
Maine to spend 3% on special education; Colorado might expand telehealth
States’ choices generally reflect a range of local priorities: While Louisiana has carved out funds for law enforcement, Maine is dedicating 3% of its statewide share for special education programs in schools, and Colorado has allocated 10% to addiction infrastructure, like workforce training, telehealth expansion, and transportation to treatment.
Maine requires that some funds be used for special education because school districts also sued the opioid companies, said state Attorney General Aaron Frey.
Patricia Hopkins said she signed on to the lawsuit because she’s seen the impact of the opioid crisis on students over the past decade as superintendent of school district 11, a rural part of central Maine’s Kennebec County with 1,950 students.

Patricia Hopkins is superintendent of a rural school district in Maine’s Kennebec County, which signed on to a lawsuit against opioid companies. She hopes the settlement funds will allow her to hire more social workers to help children whose families have been affected by the opioid crisis.
Elisha Morris
hide caption
toggle caption
Elisha Morris

Patricia Hopkins is superintendent of a rural school district in Maine’s Kennebec County, which signed on to a lawsuit against opioid companies. She hopes the settlement funds will allow her to hire more social workers to help children whose families have been affected by the opioid crisis.
Elisha Morris
A report compiled by Hopkins’ staff in 2019 showed nearly 4% of students had a parent dealing with addiction.
Sixty miles north, in rural Penobscot County, school district 19 social worker Meghan Baker said she knows two siblings who were home when first responders arrived to revive their parents with naloxone, and another set of siblings who lost their mother to an overdose.
Students who experience this trauma often become angry, act out at school and find it difficult to trust adults. When Baker refers them to counseling services in the community, they encounter waitlists that run six months to a year.
“If we could hire more guidance counselors and social workers, at least we [could] help some of those kids during the school day,” she said.
It’s clear that many people have high hopes for what the billions of dollars in opioid settlement funds arriving over the next two decades can accomplish. But they have questions too, because effectively using this large pot of money requires planning and forethought.
For people like Jacqueline Lewis in Ohio, whose family has lost so much to an epidemic too long ignored, progress feels slow.

Jacqueline Lewis, son Shaun, and his 7-year-old daughter lived together in a family home in Columbus, Ohio, until this fall, when Shaun died of an overdose.
Maddie McGarvey for KHN
hide caption
toggle caption
Maddie McGarvey for KHN

Jacqueline Lewis, son Shaun, and his 7-year-old daughter lived together in a family home in Columbus, Ohio, until this fall, when Shaun died of an overdose.
Maddie McGarvey for KHN
As she tries to make do on Social Security, Lewis focuses on the positives: Her granddaughter is a happy child, and her older brother lives with them to help out. But the financial worries gnaw at her. And what if her own health falters before her granddaughter is an adult?
“I might be OK right now, but tomorrow — I never know,” she said.
KHN correspondent Rae Ellen Bichell contributed to this report. KHN (Kaiser Health News) is a national, editorially independent program of KFF (Kaiser Family Foundation).