Registered nurse Jamie Simmons speaks with a patient during an appointment at the Greater New Bedford Community Health Center in Massachusetts. The patient, whose first name is Kim, says buprenorphine has helped her stay off heroin and avoid an overdose for nearly 20 years.
Jesse Costa for KHN
hide caption
toggle caption
Jesse Costa for KHN

Registered nurse Jamie Simmons speaks with a patient during an appointment at the Greater New Bedford Community Health Center in Massachusetts. The patient, whose first name is Kim, says buprenorphine has helped her stay off heroin and avoid an overdose for nearly 20 years.
Jesse Costa for KHN
For two decades — as opioid overdose deaths rose steadily — the federal government limited access to buprenorphine, a medication that addiction experts consider the gold-standard for treating patients with an opioid use disorder. Study after study shows it helps people continue addiction treatment while reducing the risk of overdose, and death.
Clinicians who wanted to prescribe the medicine had to complete an 8-hour training. They could only treat a limited number of patients and had to keep special records. They were given a Drug Enforcement Administration (DEA) registration number starting with X, a designation that many doctors say made them a target for drug enforcement audits.
“Just the process associated with taking care of our patients with a substance use disorder made us feel like, ‘boy, this is dangerous stuff,'” says Dr. Bobby Mukkamala, who chairs the American Medical Association’s task force on substance use disorder.
“The science doesn’t support that but the rigamarole suggested that.”
That rigamarole is mostly gone. Congress eliminated what became known as the “X-waiver” in legislation President Biden signed late last year. Now begins what some addiction experts are calling a truth serum moment.
Was the X-waiver and the burdens that came with it the real reason only about 7% of clinicians in the U.S. were cleared to prescribe buprenorphine? Or was it an excuse that masked hesitation about treating addiction, if not outright disdain for these patients?
There’s great optimism among some leaders that getting rid of the X-waiver will expand access to buprenorphine and reduce overdoses. One study from 2021 shows taking buprenorphine reduces the risk by 50%. The medication is an opioid that produces much weaker effects than heroin or fentanyl and reduces cravings for those deadlier drugs.
The nation’s drug czar, Dr. Rahul Gupta, says getting rid of the X-waiver will ultimately prevent millions of deaths.
“The impact of this will be felt for years to come,” Gupta says. “It is a true historic change that, frankly, I could only dream of being possible.”
Gupta and others envision obstetricians prescribing buprenorphine to their pregnant patients, infectious disease doctors adding it to their medical tool box, and lots more patients starting buprenorphine when they come to emergency rooms, primary care clinics and rehabilitation facilities.
We are “transforming the way we think to make every moment an opportunity to start this treatment and save someone’s life,” says Dr. Sarah Wakeman, the medical director for substance use disorder at Mass General Brigham in Boston.
Wakeman says clinicians who she’s been reaching out to for the past decade are finally willing to consider treating patients with buprenorphine. Still, she knows stigma and discrimination could undermine efforts to help those who aren’t being served. In 2021, a national survey showed just 22% of people with an opioid use disorder received buprenorphine or methadone, which is another form of medication-assisted treatment.
The truth serum experiment
The truth serum experiment – what will test whether clinicians will now step up prescribing – is underway in hospitals and clinics across the country as patients struggling with addiction queue up for treatment.
One woman named Kim, 65, is among them.
Kim’s recent visit to the Greater New Bedford Community Health Center in southern Massachusetts began in an exam room with Jamie Simmons, a registered nurse who runs the center’s addiction treatment program but doesn’t have prescribing powers. NPR agreed to use only Kim’s first name to limit discrimination linked to her drug use.
Kim tells Simmons that buprenorphine has helped her stay off heroin and avoid an overdose for nearly 20 years. Kim takes a brand of the medication called Suboxone, which comes in the form of thin film-like strips she dissolves under her tongue.
“It’s the best thing they could have ever come out with,” Kim says, “I don’t think I ever even had a desire to use heroin since I’ve been taking them.”
Buprenorphine can produce mild euphoria and slow breathing but there’s a ceiling on the effects. Patients like Kim may develop a tolerance and not experience any effects.
“I don’t get high on Suboxones,” Kim says, “they just keep me normal.”
Still many clinicians have been hesitant to use buprenorphine – known as a partial opioid agonist – to treat an addiction to more deadly forms of the drug.
Kim’s primary care doctor at the health center never applied for an X-waiver. So for years Kim has bounced from one treatment program to another, seeking a prescription. When there were lapses in her access to buprenorphine, the cravings returned – an especially scary prospect now that the powerful opioid fentanyl has replaced heroin on the streets of Massachusetts, where Kim lives.
“I’ve seen so many people fall out [overdose] in the last month,” says Kim, her eyes wide, “that stuff is so strong that within a couple minutes, boom.”
Because fentanyl can kill so quickly, the benefits of taking buprenorphine and other medications to treat an opioid use disorder have increased as deaths linked to even stronger types of fentanyl rise. Buprenorphine is present in a small percentage of overdose deaths nationwide, 2.6% – virtually always with a mix of other drugs, often benzodiazepines. Fentanyl is in 94% of overdose deaths in Massachusetts.
“Bottom line is, fentanyl kills people, buprenorphine doesn’t,” Simmons says.
That reality adds urgency to Kim’s health center visit because Kim took her last Suboxone before arriving. Her latest prescription has run out. Cravings for heroin could resume tomorrow if she doesn’t get more Suboxone. Simmons confirms the dose and tells Kim that her primary care doctor may be willing to renew the prescription now that the X-waiver is not required. But Dr. Than Win has some concerns after reviewing Kim’s most recent urine test.
It showed traces of cocaine, fentanyl, marijuana and Xanax, and Win says she’s worried about how the street drugs might interact with buprenorphine.
“I don’t want my patients to die from an overdose,” Win says. “But I’m not comfortable with the fentanyl and a lot of narcotics in the system.”
Kim is adamant that she’s not intentionally ingesting fentanyl. It might have been in the cocaine she says her roommate shares occasionally. Kim says she takes the Xanax to sleep. Her drug use presents complications that many primary care doctors don’t have experience managing. Some clinicians are apprehensive about using an opioid to treat an addiction to opioids, despite compelling evidence that it saves patients’ lives.
Win is worried about writing her first prescription for Suboxone. But she agrees to help Kim stay on the medication.
“I wanted to start with someone a little bit easier,” Win says. “It’s hard for me, that’s the reality and truth.”
About half of the providers at the health center had an X-waiver when it was still required. Simmons says some of the resistance to having the waiver was rooted in stigma or misunderstanding about addiction. She urges doctors to treat addiction as they would any other disease.
“You wouldn’t not treat a diabetic, you wouldn’t not treat a patient who is hypertensive,” Simmons says. “People can’t control that they formed an addiction to an opiate, alcohol or a benzo.”
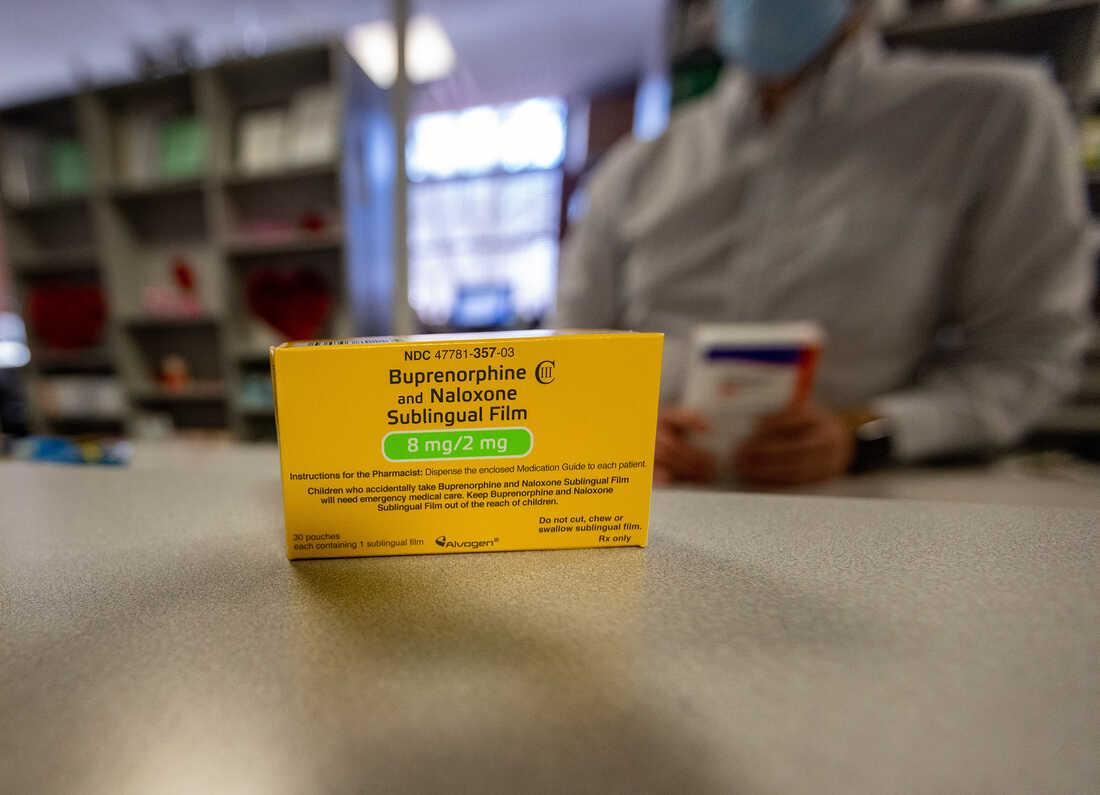
Suboxone film
Jesse Costa/WBUR
hide caption
toggle caption
Jesse Costa/WBUR
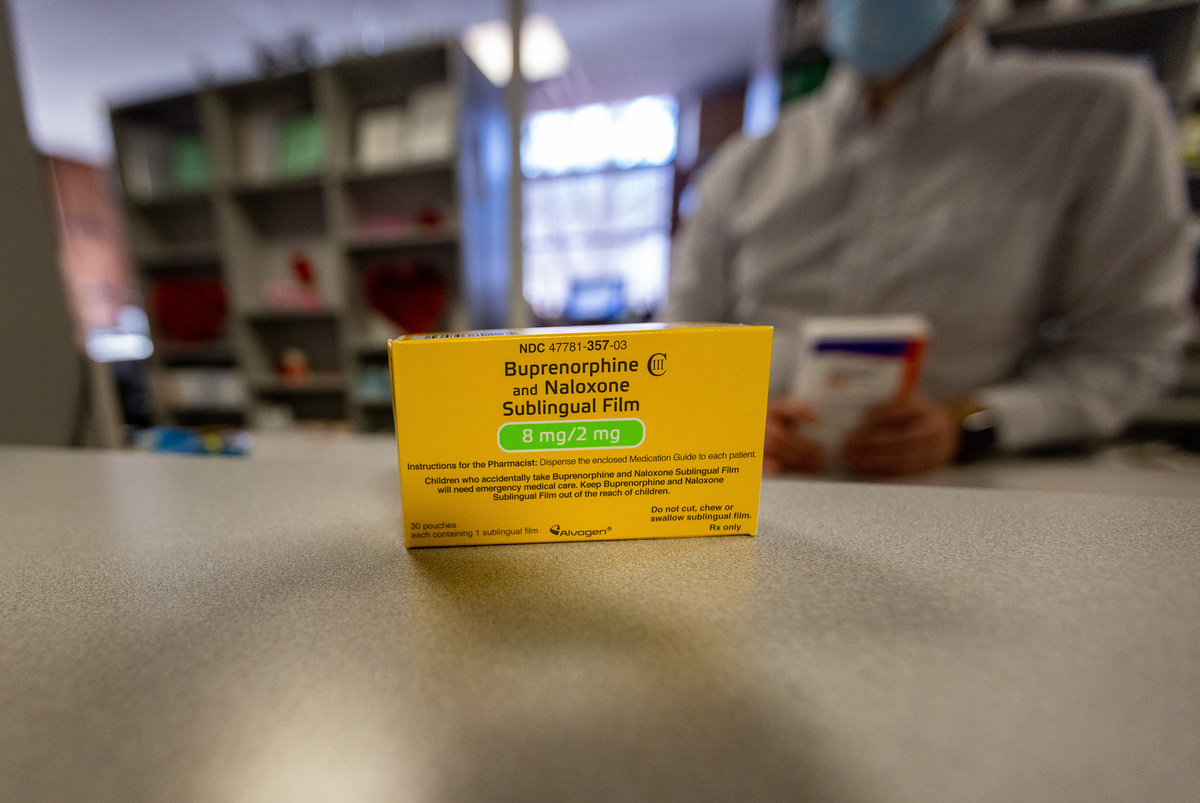
Suboxone film
Jesse Costa/WBUR
Searching for solutions to soften stigma
Although the restrictions on buprenorphine prescribing are no longer in place, Dr. Mukkamala says the perception created by the X-waiver lingers.
“That legacy of elevating this to a level of scrutiny and caution, that needs to be sort of walked back,” says Mukkamala with the AMA. “That’s going to come from education.”
Mukkamala sees promise in the next generation of doctors, nurse practitioners and physician assistants coming out of schools that have added addiction training. The AMA and the American Society of Addiction Medicine have online resources for clinicians who want to learn on their own.
Some of these resources may help fulfill a new training requirement for clinicians who prescribe buprenorphine and other controlled narcotics. It will take effect in June. The DEA has not issued details about that training.
But training alone may not shift behavior: take the experience of Rhode Island.
The number of doctors approved to prescribe buprenorphine jumped more than 200% from 2016 to 2022 after the state said physician training should include an X-waiver. Still, having the option to prescribe buprenorphine “didn’t open the floodgates” for patients in need of treatment, says Dr. Jody Rich, an addiction specialist who teaches at Brown University. The number of patients taking buprenorphine in Rhode Island increased – from 2016 to 2022 when the number of qualified prescribers jumped – but at a much slower rate .
“It all comes back to stigma,” Rich says.
He says longstanding resistance among some providers to treating addiction is shifting as younger people enter medicine. But the opioid crisis can’t wait for a generational change, he says. To expand buprenorphine access now, Rich’s research shows states could use pharmacists, partnered with doctors, to help manage the care of more patients with an opioid use disorder.
Wakeman, at Mass General Brigham, says it might be time to hold clinicians who don’t provide addiction care accountable through quality measures tied to payments.
“We’re expected to care for patients with diabetes or to care for patients with heart attack in a certain way and the same should be true for patients with an opioid use disorder,” says Wakeman.
One quality measure could be to track how often prescribers start and continue buprenorphine treatment. Wakeman says it would also help if insurers reimbursed clinics for the cost of staff who aren’t traditional clinicians but are critical in addiction care, like recovery coaches and case managers.
Will ending the X-waiver close racial gaps?
Wakeman and others are paying especially close attention to whether eliminating the X-waiver helps narrow racial gaps in buprenorphine treatment.
The medication is much more commonly prescribed to white patients with private insurance or who can pay cash. But there are also stark differences by race at some health centers where most patients are on Medicaid and would seem to have equal access to this addiction treatment.
At the New Bedford health center, Black patients represent 15% of all patients but only 6% of those taking buprenorphine. For Hispanics that comparison is 30% to 23%. Most of the health center patients prescribed buprenorphine are white, 61%, while they are just 36% of patients overall.
Dr. Helena Hansen, who co-authored a book on race in the opioid epidemic, says access to buprenorphine doesn’t guarantee that patients will benefit from it.
“People are not able to stay on a life-saving medication unless the immense instability in housing, employment, social supports — the very fabric of their communities — is addressed,” says Hansen. “That’s where we fall incredibly short in the United States.”
Hansen says expanding access to buprenorphine has helped reduce overdose deaths dramatically among all drug users in France, including those who are low-income and immigrants. There, patients with an opioid use disorder are seen in their communities and offered a wide range of social services.
“Removing the X-waiver,” says Hansen, “is not in itself going to revolutionize the opioid overdose crisis in our country. We would need to do much more.”
This story is from NPR’s partnership with WBUR and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues.